Healthcare organizations are under immense pressure to improve care quality, reduce costs, and operate more efficiently. AI is speeding and simplifying all activities and is integrated across most workflows.
But there’s a tradeoff: the moment patient data enters an AI workflow, your HIPAA obligations intensify.
HIPAA violations are not theoretical. Unauthorized access, accidental exposure through prompts, lack of auditability, or overly broad access to AI systems can all trigger compliance failures. Product managers and technology leaders must design AI workflows that assume sensitive data will flow and protect it by default.
This guide walks through a practical, product-oriented, step-by-step approach to enabling AI on healthcare data while staying aligned with HIPAA’s Technical Safeguards.
TLDR for Healthcare Product Manager
If you’re building AI in healthcare:
- Assume PHI will flow
- Design for least-privilege access
- Separate AI utility from raw data exposure
- Make authorization explicit and auditable
AI does not have to slow innovation or compromise compliance.
With the right product architecture, HIPAA-safe AI becomes an enabler, not a blocker.
HIPAA Technical Safeguards That AI Directly Impacts
Before designing the workflow, it’s important to ground ourselves in HIPAA requirements that are most affected by AI usage:
1. Access Control (§164.312(a))
HIPAA requires that only authorized individuals can access PHI.
AI systems often violate this unintentionally by:
- Exposing raw data to engineers or analysts
- Sending full PHI to LLMs or downstream tools
- Lacking fine-grained, role-based enforcement
2. Audit Controls (§164.312(b))
You must be able to record and examine activity in systems that handle PHI.
AI workflows frequently lack:
- Visibility into who accessed data
- Logs for masked vs unmasked access
- Traceability across prompts and outputs
3. Integrity Controls (§164.312(c))
PHI must not be improperly altered or destroyed.
AI pipelines that generate synthetic or inconsistent outputs can:
- Break referential integrity
- Corrupt downstream analytics
- Create compliance ambiguity
4. Transmission Security (§164.312(e))
PHI must be protected while moving between systems.
AI increases transmission risk because data flows across:
- APIs
- Model endpoints
- Agentic workflows
- Third-party tools
Example Use Case: Improving Insurance Claims Processing with AI
Let’s take a common and realistic example.
A healthcare organization wants to use AI to:
- Automatically review insurance claims
- Detect missing or inconsistent information
- Speed up approvals and reduce rework
To do this well, AI needs access to:
- Patient demographics
- Diagnosis codes
- Treatment notes
- Provider details
All of this is Protected Health Information (PHI).
Now consider who interacts with this workflow:
- Data engineers building pipelines
- ML teams tuning models
- Operations teams reviewing outputs
- Claims analysts validating exceptions
- Authorized clinicians or compliance officers
Not all of these users are authorized to see raw PHI. This is where HIPAA Technical Safeguards become critical.
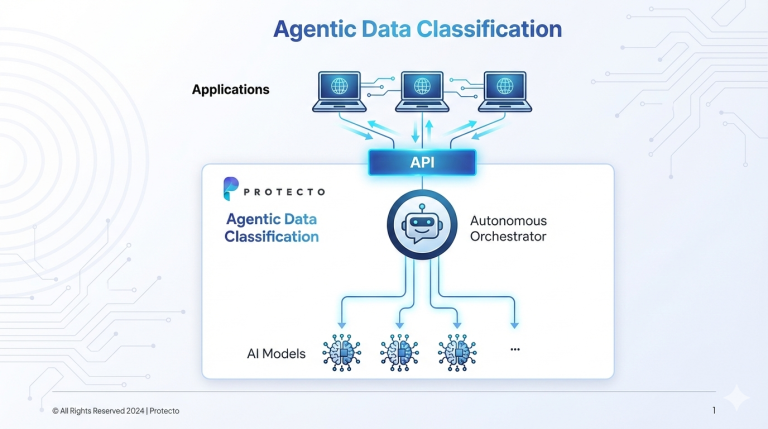
Step-by-Step: Enabling AI Safely with Protecto
Step 1: Identify PHI Before It Enters AI
The first rule of HIPAA-safe AI is simple:
Never assume downstream systems will protect sensitive data.
Protecto sits before AI systems and automatically detects PHI across:
- Structured data (claims tables, databases)
- Unstructured data (clinical notes, documents)
This ensures PHI is identified early, before it reaches models, agents, or analytics tools.
HIPAA alignment: Supports Access Control and Integrity Controls by preventing uncontrolled exposure.
Step 2: Mask PHI by Default
Once identified, PHI is deterministically masked.
Key product principles:
- Data structure is preserved
- Referential integrity is maintained, masked values remain consistent over time
- Semantic meaning and context remains intact for LLMs/agents to make decisions
This allows teams to:
- Build models, RAG or agents
- Run analytics and AI-based workflows
- Debug workflows and tune the agents
without seeing real patient data.
HIPAA alignment: Enforces Minimum Necessary access under Access Control requirements.
Step 3: Let Teams Work on Masked Data Safely
Most AI development and operations do not require raw PHI.
With Protecto:
- Engineers, analysts, and ops teams interact only with masked data
- AI models are trained and evaluated safely
- Claims processing logic runs without exposure
This dramatically reduces breach risk while accelerating development.
HIPAA alignment: Reduces blast radius and strengthens Transmission Security.
Step 4: Unmask Only for Authorized Users (Just-in-Time)
When real data is genuinely required for instance:
- Fraud team reviewing a flagged claim
- A compliance officer validating an exception
Protecto applies policy-based authorization based on the user and their role. Only then is data selectively unmasked.
Every access is logged.
HIPAA alignment: Strong Access Control + Audit Controls.
Step 5: Maintain Full Auditability Across AI Workflows
Protecto provides:
- Logs of masking and unmasking events
- User-level access trails
- Policy enforcement records
This turns AI workflows from compliance risks into auditable systems.
HIPAA alignment: Directly satisfies Audit Control requirements.
Conclusion: HIPAA-Safe AI Is a Product Decision, Not a Legal Afterthought
AI in healthcare is no longer optional. But neither is HIPAA compliance.
The biggest mistake healthcare teams make is treating compliance as something to “bolt on” after an AI system is built. In reality, HIPAA-safe AI requires intentional product architecture from day one. Architecture that assumes PHI will flow, enforces least privilege by default, and makes every access explicit, authorized, and auditable.
When designed correctly, AI does not increase compliance risk. It reduces it.
By identifying PHI before it reaches AI systems, masking data by default, enforcing policy-based access, and maintaining full auditability, healthcare organizations can unlock AI use cases without exposing patient data or slowing innovation.
HIPAA was designed to protect patients. AI, when implemented responsibly, can help healthcare teams protect both patients and productivity at the same time.
The organizations that succeed will not ask, “Can we use AI under HIPAA?”
They will design systems where safe AI is the default.